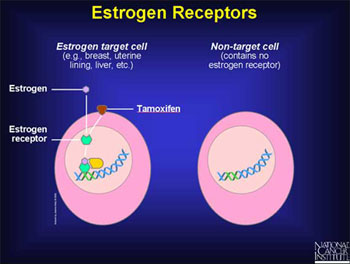
Excessive exposure to estrogen has been identified as a contributory factor for the development of endometrial cancer and breast cancer.
Etiology: the cause or origin of disease.
Extracapsular invasion: growth of cancerous tissue outside of a capsule.
Extracellular matrix: an insoluble supramolecular complex that occupies the space between cells and composed of several classes of macromolecules with specific binding interactions and spanning large distances in tissues.
Exon: a transcribed region of a gene that is present in mature messenger RNA.
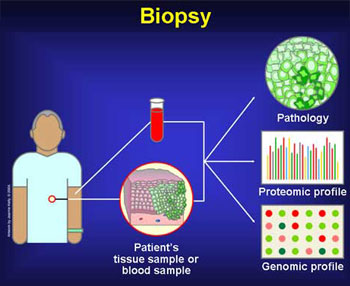
Excisional biopsy: the process of removing tissue from living patients for diagnostic examination in which the entire lesion is removed.
Experimental study: a study in which conditions are under the direct control of the investigator. In epidemiology, a study in which the population is selected for a planned trial of a regimen whose effects are measured by comparing the outcome of the regimen in the experimental group with the outcome of another regimen in a control group. To avoid bias members of the experimental and control groups should be comparable except in the regimen that is offered them. Allocation of individuals to experimental or control groups is ideally by randomization. In a randomized controlled trial, individuals are randomly allocated.
Back to the Top
Familial cancer: a form of cancer that occurs in various members of the same family at a significantly higher rate than can be expected to occur by chance.
Feedback inhibition: inhibition of an enzyme by the product of the enzyme or, in a metabolic pathway, by a product of the pathway.
Fibroblasts: a cell that produces connective tissue cells.
Fibrocytes : sameas fibroblast.
Fibrocystic disease: a term used to describe lumpy breasts. Despite the name, it is not a disease.
F.I.S.H. (fluorescence in situ hypridization): a technique involving the binding of a tagged DNA sequence to chromosomal DNA on a microscope slide and detection with fluorochrome.
Flow cytometer (also called Fluorescence Activated Cell Sorter or FACS): cells are labeled with fluorescent dye and then passed, in suspending medium, through a narrow dropping noble so that each cell is in a small droplet. A laser-based detector system is used to excite fluorescence, and droplets with positively fluorescent cells are given an electric charge. Charged and uncharged droplets are separated as they fall between charged plates, and so collect in different tubes.
Flow cytometry: a potent cell sorting method that allows several hundred to thousands of cells to be measured per second. Its uses include measurement of a cell's DNA and RNA content, from which ploidy can be determined to assess a cell population's status regarding mutations. It can also be used to separate normal and tumor cells from tissue samples and toseparate fractions of ceils in different stages of the cell cycle.
Fine needle aspiration (FNA): procedure which can be performed in the office under local anesthetic in which a skinny needle is placed into the area of abnormality and single cells removed for cytology.
Follicle: a very small excretory or secretory sac or gland.
Back to the Top
Gamete: a reproductive cell (ovum or sperm) with the haploid chromosome number.
Gene: t he functional and physical units of inheritance that are passed from parents to their offspring. The genes found in normal tissue can change their “expression”, which can give rise to cancer.
Gene amplification: an increase in the number of copies a specific gene in the cellular genome; a common genetic alteration in cancer. The proteins encoded by these amplified genes are usually expressed at high levels. Gene amplification involves an extended region of DNA often spanning several neighboring genes. Amplified genes may be located within a chromosome (usually in the form of tandem repeats) or associated with extra chromosomal circular DNA or minute chromosomal bodies.
Gene clones: an artificially created substance that is genetically identical to a chosen gene.
Gene expression: the level of activity of a gene or group of genes.
Gene expression Profile: a picture of the activity or expression of multiple genes from a single specimen.
Gene knockout: the term for the process of introducing a specific mutation into an endogenous gene to inactivate (or knockout) the gene.
Genetic instability: the inability to prevent the gain, loss and rearrangement of genomic DNA during cell division; a common genetic alteration in cancer.
Genetics: the study of genes and heredity. Heredity is the passing of genetic information and traits (such as eye color and an increased chance of getting a certain disease) from parents to offspring.
Genome: the complete DNA sequence containing the entire genetic information of an individual, a population, or a species.
Genomic instability: the recessive heritable trait associated with, but not limited to, certain DNA repair deficiencies that results in higher than normal spontaneous rates of sosmatic mutations; this trait is typically acquired by cancer cells during progression.
Genomics: the study of complex sets of genes and their effects on biology.
Genotype: the genetic constitution of an organism or virus, as distinguished from its appearance or phenotype; often used to refer to the acetic composition of one or a few genes of interest.
Germ cell: a cell that gives rise to reproductive cells.
Germ line: the cell line from which gametes are derived. Inherited (germ) cells.
Grade: a designation used for the pathologic assessment of a tumor based on the degree of cytological and architectural differentiation and number of mitoses.
Growth suppressor: a growth factor that generally inhibits cell growth.
Growth factor: a specific substance that must be present in the growth medium to permit cell multiplication.
Growth factorreceptor: a receptor (see receptor) which binds to, or responds to, a growth factor with high specificity.
Back to the Top
Half life, biological: the time required for the body to eliminate one-half of the dose of a given substance. This time is approximately the same for both stable and radioactive isotopes of any element.
Half life, radioactive: the time required for half the mass of a radioactive substance to decay into another substance. Each radionuclide has a unique half-life.
Haploid: the chromosome number of a normal gamete, with only one member of each chromosome pair. In humans, the haploid number is 23.
Haplotype: (1) a group of alleles from closely linked loci, usually inherited as a unit. (2) a set of restriction fragment lengths closely linked to one another and to a gene of interest.
Her2/Neu ( also called erb-B2): a protein involved in normal cell growth. It is found in high levels on some breast cancer cells.
Heterozygous: having one or more pairs of dissimilar alleles.
Histology: the department of anatomy that deals with the minute structure, composition, and function of the tissues.
Homologous chromosomes: chromosomes that pair during meiosis. Each homologue is a duplicate of one of the chromosomes contributed at syngamy by the mother or father. Homologous chromosomes contain the same linear sequence of genes and as a consequence each gene is present in duplicate.
Homozygous: having identical rather than different alleles at one or more loci in homologous chromosome segments.
Hormonal cancer therapy: medications used to reduce the effect of hormones in the body. In many cases of breast cancer, hormones can fuel the growth of breast cancer. Common hormonal therapies include tamoxifen and a newer class of drugs called aromatase inhibitors. Hormonal therapies are used to treat women with estrogen receptor-positive breast cancer.
Hormone Receptor: A protein on the surface of a tumor cell that binds to a certain hormone, activating tumor growth.
Hormonal replacement therapy (HRT): hormones (estrogen, progesterone, or both) given to women after menopause to replace the hormones no longer produced by the ovaries.
Human Genome Project: an international research and technology-development effort aimed at mapping and sequencing the entire genome of human beings.
Hyperplasia: an overgrowth of cells.
Back to the Top
Incidence: the number of instances of illness commencing during a given period in a specified population.
Incisional biopsy: surgical biopsy in which only a portion of the area of abnormality is removed.
Independent: assortment random distribution of unlinked genes into gametes, as with genes in different (nonhomologous) chromosomes.
Immunohistochemistry: department of chemistry that deals with the substances and reactions concerned in immunity as it relates to the microscopy of the tissue.
Immunosuppression: the inhibitions or restriction of the normal functioning of the immune system.
Inert: having no action.
Initiator: a molecule which initiates replication once it binds to replicators.
Insertion: the addition of one or more base pairs into a DNA molecule.
In situ: early stage breast cancer characterized by cells showing changes indicative of cancer but without evidence of invasion and metastasis.
Interaction: differences in the effects of one or more factors according to the level of the remaining factor(s).
Interferon: a class of small soluble proteins produced by lymhoid as well as nonlymhoid cells that are capable of affecting protein synthesis and cell-mediated immunity.
Interleukin: one of a group of immunologic cytokines that as originally defined indicated a cytokine synthesized by one type of immunologic cell and affecting another type or group of immunologic cells; now frequently recognized to function as cytokines as well by affecting the function of cells other than those in the immune system.
Intrinsic resistance: the resistance of previously untreated tumors to chemotherapy.
Invasive: referring to cancer cells that have spread beyond normal boundaries.
Invasive carcinoma (IC): a cancer that sends projections into the stroma. They can be of the ductal (IDC) or lobular (ILC) types, depending on the morphology of the cancer.
Inversion: a chromosomal rearrangement in which a segment of a chromosome is reversed end to end.
In vitro: research testing done in the test tube.
In vivo: research testing done in animals.
Back to the Top
Ki 67: degree of proliferation.
Kinase: any enzyme that transfers a phosphates group from a nucleoside triphosphate to another molecule.
Knockout mouse: a laboratory mouse from which a specific gene has been genetically deleted (“knocked out”) usually by homologous recombination.
Back to the Top
Lateral: denoting a position more toward the side.
Lead time bias: overestimation of survival time, due to backward shift in the starting point for measuring survival that arises when diseases such as cancer are detected early, as by screening procedures.
L.C.I.S.: lobular carcinoma in situ.
Ligand: a molecule that will bind to a complementary site on a given structure. For example, oxygen is a ligand for hemoglobin and a substrate of an enzyme molecule is a specific ligand of that molecule.
Linkage: genes on the same chromosome show linkage if they have a tendency to be transmitted together through meiosis.
Lipids: any of a group of fats and fat like substances including fatty acids, neutral fats, and steroids that contain aliphatic hydrocarbons, are water insoluble, and serve as a source of energy for the body.
Liposomes: a synthetic membrane vesicle made from phospholipids and used for in vitro study of membrane-defined events such as transport, or for the delivery of substances to a cell.
Lobule: a subdivision of the lobes of the breast. Cancer that begins in a lobule is called lobular carcinoma.
Local Recurrence: the reappearance of cancer in the part of the body where it first occurred.
Locus: the position of a gene on a chromosome. Different forms of the gene (alleles) may occupy the locus.
Lumpectomy: removal of the lump as well as a margin of normal tissue around it that usually refers to removal of a cancerous tumor, although some also use it loosely to describe removal of benign tumors.
Lymph node dissection: when the surgeon removes several lymph nodes during either a mastectomy or lumpectomy so that the pathologist can then dissect the node into thin slices that are then stained and examined under the microscope to look for cancerous cells.
Lymphatic system: the tissues and organs that produce, store and transport cells that fight infection and disease.
Back to the Top
Macrophage cells: cells that have left the bone marrow and blood stream to settle in an area of tissue where it fulfills several important immune functions in both the cellular and humoral arms.
Mammary: all “mammals” have “mammary” glands that produce milk to nurse their young.
Mammary chain lymph nodes: all mammals have a chain of mammary glands running down their chest (in humans only one gland on each side of the breast develops; following the chain of mammary glands are a chain of lymph nodes.)
Mammography: an x-ray technique used to image the soft tissues of the breast. Breast images are generated using low-voltage x-rays to demonstrate tissue density differences. Tumors, having higher density than normal tissues, are offset from surrounding tissues in a mammogram. The detection limit for current state-of-the-art mammography devices is approximately 1-2 mm for lesions with significant calcification. Because mammography is associated with a relatively high false-positive rate and is often unable to distinguish between benign and malignant lesions, the identification of a suspicious mammographic feature is usually followed by needle localization or various biopsy techniques.
Margins: an area next to and around a tumor. It is important to have “clean margins” after surgical procedures to remove abnormal cells.
Marker: a gene that has a known location on the chromosome and an established phenotype and that thus can be used as a reference to study or locate another gene of interest.
Mastectomy: removal of the breast.
Mastectomy, radical: removal of the nipple, breast tissue, axillary lymph nodes, as well as underlying pectoralis muscle.
Mastectomy, modified radical: removal of the nipple, breast tissue and lymph nodes. Total (simple) mastectomy is removal of the nipple and breast tissue.
Mastectomy, subcutaneous: removal of breast tissue except for the nipple that has been shown to leave additional breast tissue around the periphery.
Meiosis: the special type of cell division occurring in the germ cells by which gametes containing the haploid chromosome number are produced from diploid cells. Two meiotic divisions occur: meiosis I and meiosis 11. Reduction in number takes place during meiosis 1. Not to be confused with mitosis.
Menopause: end of the menstrual cycle usually occurring between the ages of 40-55. Ovarian function is reduced and estrogen secretion decreases or stops.
Meta-analysis: a combination of the prefix "meta" used in the sense of later or more highly organized or specialized form of' with the word analysis. Refers to the qualitative and quantitative analysis of one or
more previous clinical studies usually involving pooling of data across studies.
Metastasis: spread of cancer out of organ of origin to distant areas.
Microcalcifications: tiny deposits of calcium in the breast that can show up on a mammogram. Certain patterns of microcalcifications are sometimes a sign of breast cancer.
Microinvasions: invasions of cancer cells that are too few in number to be detected.
Micrometastasis: metastasis too small to measure with current technology due to a small number of cells.
Mitogenic signal: a signal to produce or stimulate cellular proliferation.
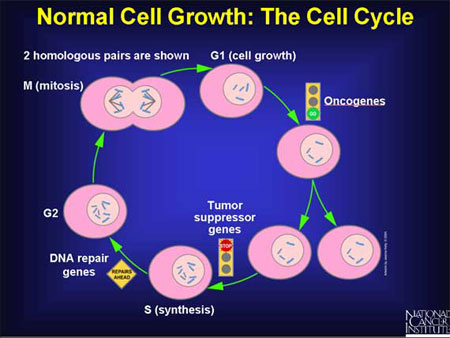
Mitosis: the process of ordinary cell division resulting in the formation of two cells genetically identical to the parent cell. Not to be confused with meiosis.
Monoclonal antibodies: a type of protein made in the laboratory that can locate and bind to substances in the body, including tumor cells.
Mosaic: an individual or tissue with at least two cell lines differing in genotype or karyotype derived from a single zygote. Not to be confused with chimera.
mRNA (messenger RNA): see RNA.
Mutagen: a physical or chemical agent which raises the frequency of mutation above the spontaneous rate.
Mutation: any permanent heritable change in the sequence of genomic DNA.
Back to the Top
Necrosis: acute cell death in conditions that cause the collapse of cellular integrity.
Needle localization: process of introducing a thin wire into the breast under mammography or ultrasonic guidance to pinpoint suspected minimal breast cancers.
Neoplasia: the process of tumor formation; the proliferation of cells under conditions that would not elicit similar growth in normal cells.
Neoplasm: the process of tumor formation; a tumor.
Neurogenic: originating in the nervous system.
Nucleotide: a molecule composed of a nitrogenous base, a 5-carbon sugar, and a phosphate group.
Nucleus: the center of the cell; the organelle bounded by a membranous envelope that contains the chromosomes in a eukaryotic celi.
Back to the Top
Observational study: epidemiologic study in situations where nature is allowed to take its course; changes or differences in one characteristic are studied in relation to changes or differences in other(s), without the intervention of the investigator.
Off –label drug use: use of an FDA- approved drug by a physician to treat a disease other than that for which the drug was approved.
Oncogene: a dominantly acting gene involved in unregulated cell growth and proliferation responsible for tumor development. Mutation, overexpression, or amplification of oncogenes in somatic cells may lead to cancerous (neoplatic) transformation. Contrast with proto-oncogene and tumor suppressor gene.
Oncotype DX®: a unique diagnostic test that looks at the genomic profile of a breast tumor to quantify the likelihood that early-stage, estrogen receptor-positive, lymph node-negative breast cancer will return, or recur (distant recurrence), and provide information about a woman's likely benefit from chemotherapy (commonly used drugs to treat early-stage breast cancer).
Open label trial: 1. A nonmasked drug research study (trial). 2. Any nonmasked trial.
Oral contraceptives: birth control pills.
Back to the Top
P: a term used to designate the short arm of the chromosome.
P53: a tumor suppressor gene that is the most frequently mutated gene known to date in human cancers. Its loss of function leads to daughter cells with genomic instability and predisposition to tumor development. Functional loss of p53 also blocks a major apoptotic pathway. Certain p53 mutants can act, moreover, as directly transforming oncogenes.
P53 mouse a mouse that has been genetically engineered to be devoid of functional p53 or to express mutant alleles that inhibit wild-type p53 function.
Palpable: able to be felt.
Parafin block: a purified mixture of hydrocarbins obtained from petroleum which is more or less translucent. Used to imbed tissue so as to keep it in a permanent block. Slices of this block can be cut years later with no change in microscopy.
PCR (polymerase chain reaction): a technique in which a short DNA or RNA sequence can be amplified 106 times by means of two flanking oligonucleotide primers and repeated cycles of amplification with a polymerase. Permits analysis of a short sequence from very small quantities of DNA or RNA without the necessity of cloning it first.
Pedigree: a diagram setting forth the ancestral history or genealogical register.
Phase I trial: the first stage in testing a new drug in humans. Performed as part of an approved Investigational New Drug Application under Food and Drug Administration guidelines. The studies are usually done to generate preliminaryinformation on the chemical action, toxicity, and safety of the drug. Usually done without a comparison group.
Phase II trial: the second stage in testing a new drug in humans. Performed as part of an approved Investigational New Drug Application under Food and Drug Administration guidelines. Generally carried out on patients with the disease or condition of interest. The main purpose is to provide preliminary information on treatment efficacy and to supplement information on safety obtained from phase I trials. Usually, but not always, designed to include a control treatment and random allocation of patients to treatment.
Phase III trial: the third and usually final stage in testing a new drug in humans. Performed as part of an approved Investigational New Drug Application under Food and Drug Administration guidelines. Concerned primarily with assessment of dosage effects and efficacy and safety. Usually designed to include a control treatment and random allocation to treatment. Depending upon the results of this phase, the drug manufacturers may request permission to market the drug by submission of a New Drug Application to the Food and Drug Administration.
Phase IV trial: generally, a randomized controlled trial that is designed to evaluate the long-term safety and efficacy of a drug for a given indication and that is done with Food and Drug Administration approval. Usually carried out after censure of the drug for that indication.
Phenotype: the observed biochemical, physiological, and morphological characteristics of an individual, as determined by his or her genotype and the environment in which it is expressed. Also, in a more limited sense, the expression of some particular gene or genes.
Phosphate: the molecule forming the backbone of a DNA molecule. It contains atoms of phosphorus and oxygen.
Placebo: an inactive substance or procedure given as a substitute for an active medication or procedure that is intended to provide baseline measurements in a research study.
Ploidy: the state of a cell with respect to the number of genomes it contains. Gametes (i.e., sperm, egg, germ cells) normally contain a single set of chromosomes (one genome) and are haploid. Somatic cells normally contain two sets of chromosomes (two genomes) and are diploid. Abnormal cells not containing an exact multiple of the haploid number of chromosomes, indicative of genetic mutations, are anueploit.
Polypeptide: chain a polymer of amino acids linked together by peptide bonds.
Polyploidy: the condition of a cell or organism with more than two complete sets of chromosomes.
Polysomy: the condition of a diploid cell or organism having three or more copies of a particular chromosome.
PR (Progesterone Receptor): a protein that may be present on certain cells to which progesterone molecules can attach. The term “PR positive” refers to tumor cells that contain the progesterone receptor protein. These cells are generally sensitive to hormone therapy.
Precursor cell: a cell that is less differentiated than its progeny.
Predictive marker: a test that may be able to predict cancer.
Prognostic marker: a test which may afford an indication as to prognosis or outcome.
Premenopausal: before the menopause.
Pre-neoplastic: before the development or existence of a tumor.
Prevalence: the number of instances of a given disease or other condition in a given population at a designated time.
Progestins: the name used for certain brands of synthetic progesterone.
Progression: the ability of transformed cells to proliferate and expand into a large primary tumor population.
Proliferate: an increase in cell number by the process of cell division. Healthy cells proliferate, but self-correct any errors. Unhealthy cells are those that have not self-corrected and continue to divide and multiply with errors.
Promoter DNA: sequences located in the 5' end of a gene that determine the site of initiation of transcription and the quantity and sometimes the tissue distribution of mRNA.
Protease: an enzyme that digests proteins.
Protein: a molecule composed of one or more polypeptide chains.
Proto-oncogene: a normal gene involved in some aspect of cell division or proliferation, which if activated by a mutational event, is capable of becoming an oncogene.
Protoplasm: the substance within the plasma membrane of the cell.
Back to the Top
Quadrantectomy: removal of 1/4 of the breast tissue.
Back to the Top
Rad: a measurement of radiation absorbed by tissues. Acronym for “radiation absorbed dose”.
Radiation: usually consisting of high voltage x-rays, radiation kills dividing cells by inducing DNA damage. Because cancer cells divide more frequently than normal cells, radiation kills a larger proportion of cancer cells.
Randomization: allocation of individuals to groups for experimental and control regimens by chance. Within the limits of chance variation, randomization should make the control and experimental groups similar at the start of an investigation and ensure that personal judgement and prejudices of the investigator do not influence allocation.
Randomized controlled trial (RCT) (also called randomized clinical trial, randomized control trial, randomized controlled clinical trial): an experiment in which people are randomly allocated into groups, usually called "test" and "control" groups, to receive or not to receive an experimental preventive or therapeutic procedure, maneuver, or intervention. The results of outcomes of both groups are then compared. RCTs are generally regarded as the most scientifically rigorous method of hypothesis research testing available in epidemiology.
Receptor: a molecule that binds to, or responds to something else more mobile, with high specificity. Many receptors are membrane-bound, though others are free in the cytosol. Receptors are highly specific for certain ligands.
Recessive gene: in diploid organisms a gene which is phenotypically manifest in the homozygous state but is masked in the presence of its dominant allele. Usually the dominant gene produces a functional product, while its recessive allele does not.
Recombinant DNA: a DNA molecule constructed from segments from more than one parental DNA molecule.'
Recombination: the formation of new combinations of linked genes by crossing over between their loci.
Recurrence: a return of the cancer after an initial diagnosis and treatments that removed evidence of disease for a period of time.
Reduction division: the first meiotic division, so called because at this stage the chromosome number per cell is reduced from diploid to haploid.
Regulatory gene: a gene with the primary function of controlling the rate of synthesis of the products of one or more other genes.
Replication: the duplication of a DNA molecule during which both strands are used as templates.
Replicator: a genetic element which behaves as an autonomous unit during DNA replication.
Ribosomes: extremely small structures in the cell made from a type of RNA. They attach to messenger RNA and read the genetic code during protein synthesis.
Ring chromosome: a structurally abnormal chromosome in which the end of each chromosome arm has been deleted and the broken arms have reunited in ring formation.
Risk: the risk of developing a disease is usually described in terms of relative risk. Relative risk is calculated by dividing the frequency of mortality in a group exposed to a carcinogen by the frequency of mortality in an unexposed group.
Risk factor: an aspect of personal behavior or lifestyle, an environmental exposure, or an inborn or inherited characteristic that on the basis of epidemiologic evidence is known to be associated with health related condition(s) considered important to prevent.
RNA (ribonucleic acid): a nucleic acid that is a universal component of all living cells transmitting genetic messages from DNA to the cell.
Back to the Top
Sarcoma: cancer that arises from connective tissue such as bone, cartilage, or muscle.
Segmentectomy: removal of a segment of breast tissue; usually the same as lumpectomy.
Screening: looking for masses or suspicious areas in breast tissue on a periodic basis.
Signaling (cell signaling): release by one cell of substances that transmits information to other cells.
Single-blind(ed): a condition where certain persons (e.g. the study physicians) are informed of some aspect of a clinical trial (research study), whereas other persons (e.g. patients) are purposefully not told that information.
Staging: a classification system for breast cancer based on the size of the tumor, whether the cancer has spread to the lymph nodes, and whether the cancer has spread to other sites in the body (metastasis).
Stem cell: the most undifferentiated cell of a lineage.
Stromal cell: connective tissue cells that support and nourish the functional tissues of an organ or structure. Stromal cells can interact with stem cells to reduce the probability of apoptosis in the stem cells.
Spicules: a sharp needle like structure in the nucleus of cells.
Substrate: a specific substance acted on by an enzyme.
S ubstitution: the replacement of one or more base pairs in a DNA molecule.
Systematic review: see meta-analysis.
Back to the Top
Tamoxifen: a medication that interferes with the activity of the hormone estrogen. Tamoxifen is used to treat women with estrogen receptor-positive breast cancer.
Transcription: the synthesis of a single stranded RNA molecule from a DNA template in the cell nucleus, catalyzed by RNA polymerase.
Transcription factor: a protein required for recognition by RNA polymerases of specific stimulatory sequences in eukaryotic genes.
Transformation: any alteration in the properties of a cell which is stably inherited by its progeny. Transformation usually refers to malignant transformation, which is a change in animal cells in culture which usually greatly increases their ability to cause tumors when injected into animals.
Translation: the synthesis of a polypeptide from its mRNA template.
Translational research: a term used to describe the process by which the results of research done in the laboratory are used to develop new ways to diagnose and treat disease.
Translocation: the transfer of a segment of one chromosome to another chromosome. If two nonhomologous chromosomes exchange pieces, the translocation is reciprocal.
Transduction: see signal transduction.
Treatment Monitoring: an ongoing and frequent assessment by the medical team, during the time of treatment, to monitor how the patient is tolerating the treatment and how the cancer is responding.
Triple-blind(ed): double-masked plus masking for the individual or group of individuals responsible for treatment monitoring.
Tumor: t issue growth where the cells that make up the tissue have multiplied uncontrollably. A tumor can be benign (non-cancerous) or malignant (cancerous).
Tumor dormancy: when cancer becomes “dormant” or stops growing for a period of time.
Tumor grade: the characterization of a tumor based on how similar in appearance the cancer cells are to normal cells, and on how many of those tumor cells are dividing. Tumor grade is one of many factors that, when used in combination, can indicate how aggressive someone's cancer is.
Tumor necrosis factor (TNF): a protein made by white blood cells in response to an antigen (substance that causes the immune system to make a specific immune response) or infection. Tumor necrosis factor can also be made in the laboratory. It may boost a person’s immune response, and also may cause cell death (necrosis) of some types of tumor cells. Tumor necrosis factor is being studied in the treatment of some types of cancer. It is a type of cytokine.
Tumor stage: the status of cancer based on the size of the tumor, whether it has spread to the lymph nodes, and whether it has spread to other sites in the body (metastasis).
Tumor suppressor gene: a normal gene involved in the regulation of cell growth. Recessive mutations can lead to tumor development, as in the retinoblastoma gene or the p53 gene.
Back to the Top
Western Blot: a technique for identifying a specific protein and its molecular weight by gel electrophoresis and specific antibody.
Wild type: the usual or typical form of an organism in nature as compared to a mutated form.
Wire localization: another name for needle localization.
Zygote: diploid cell resulting from the fusion of male and female gametes at fertilization.
Back to the Top