What information does a pathology report usually include?
Although pathology reports are written by physicians for physicians, you may be able to decipher some of the medical jargon provided by the report.
The structure and information provided in your pathology report may vary, but the following sections are usually included:
Demographics: This section includes your name and date of procedure. You should check that this information is correct to ensure that you have the correct pathology report.
Specimen: The specimen section describes the origin of the tissue sample(s)
such as what
part of your body did it come from.
Clinical History: The clinical history section provides a brief description of your medical history relevant to the tissue sample that the pathologist is examining.
Clinical Diagnosis (Pre-Operative Diagnosis): The clinical diagnosis describes what the doctors are expecting before the pathologic diagnosis.
Procedure: The procedure describes how the tissue sample was removed.
Gross Description (Macroscopic): The gross description includes the pathologist’s observations of the tissue sample using the naked eye. It may include size, weight, color or other distinguishing features of the tissue sample. If there is more than one sample, this section may designate a letter or number system to distinguish each sample.
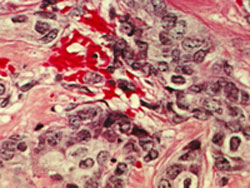
Microscopic Description:
In the microscopic description, the pathologist describes how the cells of the tissue sample appear under a microscope.
- Cell Structure: assigns a histologic grade to the tumor. The histologic grade helps the pathologist identify the type of tumor.
The grade may be described numerically with the Scarff-Bloom-Richardson system (1-3) or as well-differentiated, moderately-differentiated or poorly differentiated.